COVID-19’s Unconventional Seasonal Patterns
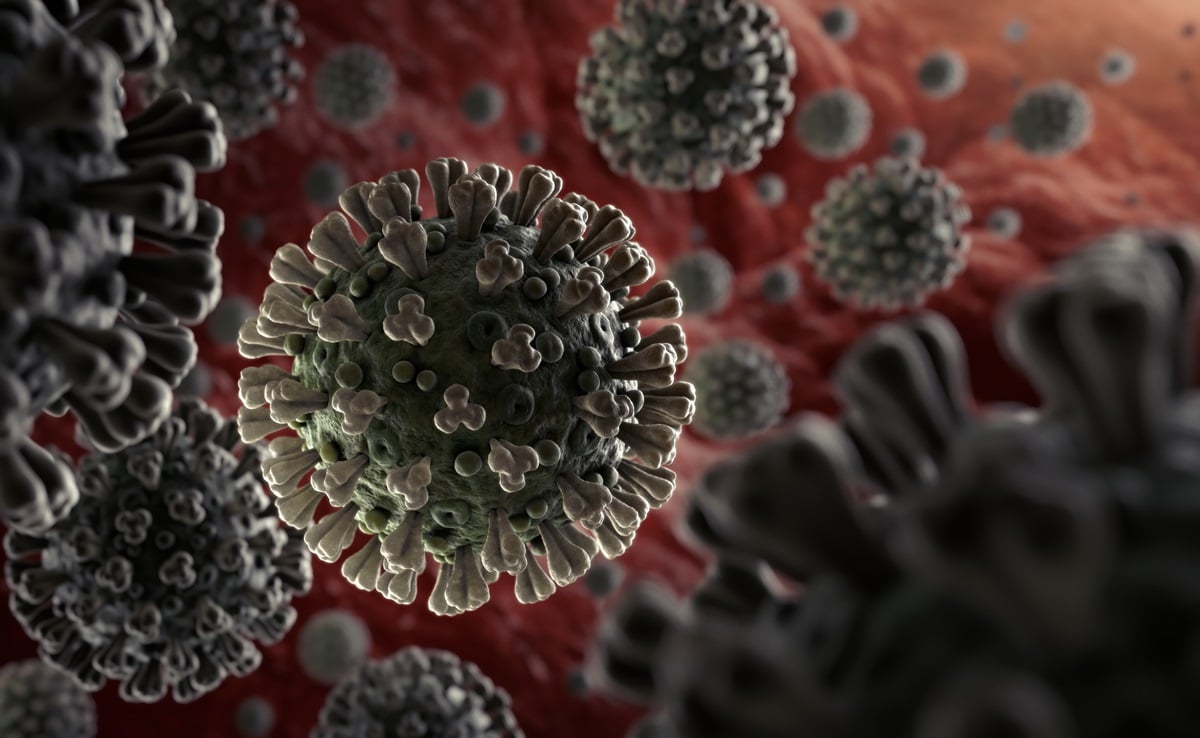
While many people believe that the COVID-19 pandemic is over, scientists studying the disease have noticed that it has not yet fallen into a predictable seasonal pattern like most respiratory pathogens. Influenza and other respiratory viruses tend to strike during specific seasons, such as winter or fall, but this has not been the case for SARS-CoV-2, the virus that causes COVID-19.
Factors Affecting COVID-19 Seasonality
Although you can contract these viruses at any time of the year, transmission typically increases during their respective seasons. It was expected that SARS-CoV-2 would eventually follow a similar pattern once human immune systems and the virus reached a sort of balance. However, experts have noted that the virus has not yet exhibited clear seasonality.
Kanta Subbarao, the director of the World Health Organization’s Collaborating Centre for Reference and Research on Influenza, expressed the lack of a clear seasonal pattern for SARS-CoV-2. Michael Osterholm, the director of the Center for Infectious Disease Research and Policy at the University of Minnesota, agreed, stating that the virus does not currently have a definable pattern but could develop one in the future.
Variants and their Impact on Transmission Patterns
Maria Van Kerkhove, the World Health Organization’s technical lead for COVID-19, believes that there are hints of a transmission pattern known as “periodicity” or waves of infection occurring every five to six months in different populations. However, this pattern is not consistent on a national or hemispheric level. The absence of seasonality in COVID-19 has practical implications. Knowing when to expect disease surges is crucial for health care planning and the timing of booster shots. The efficacy of vaccines against COVID-19 diminishes over time, so administering booster shots at the appropriate moments is essential.
Van Kerkhove suggests that waning immunity in the population contributes to periodic increases in transmission. Protection against severe disease remains relatively strong, but protection against basic infection is short-lived, as seen with other human coronaviruses. Reinfection can occur within a year, or even as soon as six months, after a previous infection.
While some experts, like infectious diseases epidemiologist Michael Mina, believe that SARS-CoV-2 has been displaying seasonal behavior to some extent, others, such as Ben Cowling, an infectious diseases epidemiologist at the University of Hong Kong, think that it is still in the process of developing a seasonal pattern.
The Role of Environmental Factors in Virus Transmission
The emergence of new variants such as Beta, Delta, and Omicron has been linked to the patterns of COVID-19 infections in the spring, summer, and late autumn of 2021. These patterns are not influenced by environmental conditions. Instead, they are believed to be influenced by the “force of infection,” which allows the virus to spread even during times when it normally wouldn’t be able to. This force also affects the transmission of other pathogens like the flu and RSV.
The reasons behind the seasonality of viruses are still not completely understood, but it is thought to be a combination of factors including human activities such as schools and holiday travel, as well as environmental factors like temperature and humidity. In colder winters, the lack of humidity in the air weakens mucus membranes, making it easier for viruses to survive outside of a human host. Furthermore, people in temperate climates tend to gather indoors during the winter, which can lead to suboptimal air quality and increased transmission. In tropical climates, where transmission occurs year-round, there are no defined flu seasons like those seen in temperate zones. Climate variables, especially temperature and humidity, play a significant role in the survival and transmission of pathogens.